This page shall be updated regularly upon discovery of research that fits the following parameters: research relating to the connection between acetaminophen and autism.
Please use the following page not as a conclusive finality to the scientific research available on the connection between acetaminophen and autism, but as a way of informing yourself and the public that there are environmental factors associated with autism, and that the question ‘is autism genetic?’ deserves careful scrutiny.
It is my present hypothesis that if a factor associated with autism in human studies is also inducing autism-like traits in animal studies with zero exposure to other toxins, then the toxin may be capable of inducing autism alone in humans prior to factoring co-exposure to other toxins.
How to Interpret the Numbers on this Page
When you browse various pages on toxins, you’ll encounter many studies. There will be a research paper title followed by numbers underneath. What do those numbers mean and why are there so many of them?
Here’s what those numbers signify:
- 1 = No Difference Between Groups: If the number is 1, it means there’s no difference in the likelihood of developing the condition (like autism) between the group exposed to a certain factor and the group that wasn’t.
- Greater than 1 = Increased Likelihood: If the number is greater than 1, it indicates that the group exposed to the factor has a higher likelihood of the condition. For example:
- 1.5: This means the exposed group has 1.5 times the odds or risk of developing autism compared to the non-exposed group. In other words, their risk is 50% higher.
- Less than 1 = Decreased Likelihood or Protective Effect: Numbers less than 1 suggest that exposure might reduce the likelihood of the condition or could even be protective. For instance:
- 0.75: This would mean the exposed group has 25% lower odds or risk compared to those not exposed.
- Multiple Numbers and Analyses:
- You’ll notice multiple numbers because researchers often look at different aspects related to autism, not just diagnosis but also symptoms or associated traits. They might also adjust for other factors (like age, gender, other health conditions) to isolate the effect of the factor they’re studying. This is why you see various analyses:
- Raw Data: Initial numbers before adjustments.
- Adjusted Analyses: Numbers after accounting for other variables to see if the factor still has an effect.
- You’ll notice multiple numbers because researchers often look at different aspects related to autism, not just diagnosis but also symptoms or associated traits. They might also adjust for other factors (like age, gender, other health conditions) to isolate the effect of the factor they’re studying. This is why you see various analyses:
Thus, when you see a number like 1.5, think of it as “the risk or odds of autism for the exposed group is 1.5 times higher compared to those not exposed.” This doesn’t mean everyone exposed will develop autism, but rather, their risk is increased by that factor.
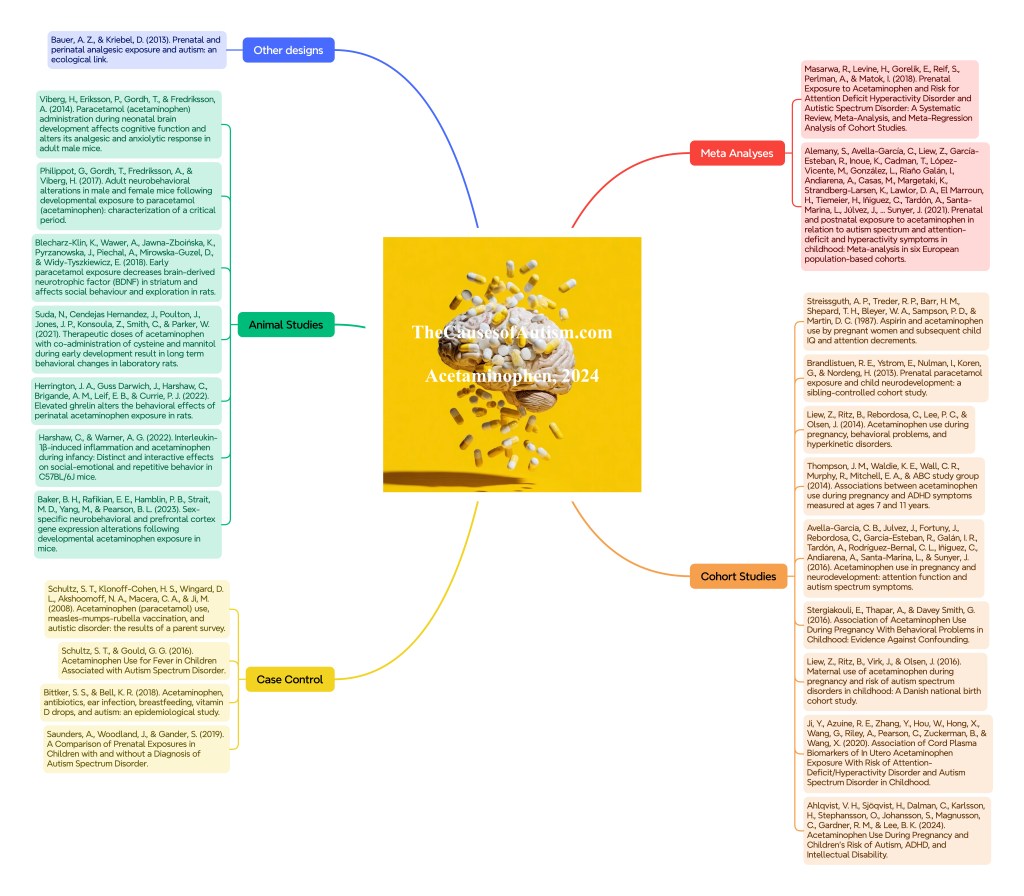
Meta Analyses
- Masarwa, R., Levine, H., Gorelik, E., Reif, S., Perlman, A., & Matok, I. (2018). Prenatal Exposure to Acetaminophen and Risk for Attention Deficit Hyperactivity Disorder and Autistic Spectrum Disorder: A Systematic Review, Meta-Analysis, and Meta-Regression Analysis of Cohort Studies. American journal of epidemiology, 187(8), 1817–1827. https://doi.org/10.1093/aje/kwy086
- Autism and emotional problems- 1.19x Risk Ratio
- Sensitivity Analysis (without Streissguth study)- 1.19x Risk Ratio
- Sensitivity Analysis (without Brandlistuen study)- 1.19x Risk Ratio
- ADHD- 1.34x Risk Ratio
- Sensitivity Analysis (without Streissguth study)- 1.39x Risk Ratio
- Sensitivity Analysis (without Brandlistuen study)- 1.34x Risk Ratio
- Hyperactivity- 1.24x Risk Ratio
- Conduct Disorder- 1.23x Risk Ratio
- Covariates: mean age of child at follow-up, maternal fever, maternal age at birth, maternal smoking, maternal socioeconomic status, latitude of country, NOS score, and duration of exposure to acetaminophen.
- Significant Moderators
- Children’s age at follow up- β = 0.03, 49% heterogeneity explained
- Meaning: Association was greater in studies with older age at follow-up
- Duration of exposure- β = 0.00, 99% heterogeneity explained
- Association was greater in studies with longer duration of exposure to acetaminophen
- Maternal Age- β = −0.17, 99% heterogeneity explained
- Association was decreased in studies with younger maternal age
- Children’s age at follow up- β = 0.03, 49% heterogeneity explained
- Autism and emotional problems- 1.19x Risk Ratio
- Alemany, S., Avella-García, C., Liew, Z., García-Esteban, R., Inoue, K., Cadman, T., López-Vicente, M., González, L., Riaño Galán, I., Andiarena, A., Casas, M., Margetaki, K., Strandberg-Larsen, K., Lawlor, D. A., El Marroun, H., Tiemeier, H., Iñiguez, C., Tardón, A., Santa-Marina, L., Júlvez, J., … Sunyer, J. (2021). Prenatal and postnatal exposure to acetaminophen in relation to autism spectrum and attention-deficit and hyperactivity symptoms in childhood: Meta-analysis in six European population-based cohorts. European journal of epidemiology, 36(10), 993–1004. https://doi.org/10.1007/s10654-021-00754-4
- Autism Spectrum Condition (ASC)
- ASC + Prenatal Exposure (Overall Random Effects Model)- 1.19x Odds Ratio
- Boys- 1.28x Odds Ratio
- Danish National Birth Cohort (DNBC) Hospital Diagnosis- 1.16x Odds Ratio
- ASC + Prenatal Exposure (Overall Random Effects Model)- 1.19x Odds Ratio
- ADHD
- ADHD + Prenatal Exposure (Overall Random Effects Model)- 1.21x Odds Ratio
- Boys- 1.23x Odds Ratio
- DNBC Hospital Diagnosis- 1.3x Odds Ratio
- ADHD + Prenatal Exposure (Overall Random Effects Model)- 1.21x Odds Ratio
- Sensitivity Analyses
- ASC (Excluding ADHD cases)- 1.16x Adjusted Odds Ratio
- Boys + ADHD Symptoms and Diagnosis- 1.31x Adjusted Odds Ratio
- Girls + ADHD Symptoms and Diagnosis- 1.39x Adjusted Odds Ratio
- Adjusted for Additional Covariate Analysis (chronic diseases, use of other drugs and use of folic acid)
- ASC Symptoms- 1.21x Adjusted Odds Ratio
- ASC Symptoms + Diagnosis- 1.18x Adjusted Odds Ratio
- ADHD Symptoms- 1.22x Adjusted Odds Ratio
- ADHD Symptoms and Diagnosis- 1.33x Adjusted Odds Ratio
- Individual Questionnaires
- ALSPAC
- ASC Symptoms- 1.24x Adjusted Odds Ratio
- ADHD Symptoms- 1.23x Adjusted Odds Ratio
- DNBC, ADHD Symptoms- 1.19x Adjusted Odds Ratio
- GASP
- ASC Symptoms- 1.2x Adjusted Odds Ratio
- ADHD Symptoms- 1.19x Adjusted Odds Ratio
- GenerationR
- ASC Symptoms- 1.16x Adjusted Odds Ratio
- ADHD Symptoms- 1.19x Adjusted Odds Ratio
- INMA
- ASC Symptoms- 1.22x Adjusted Odds Ratio
- ADHD Symptoms- 1.21x Adjusted Odds Ratio
- RHEA
- ASC Symptoms- 1.18x Adjusted Odds Ratio
- ADHD Symptoms- 1.21x Adjusted Odds Ratio
- ALSPAC
- Children’s age at outcome assessment did not modify the association between prenatal or postnatal exposure to acetaminophen and ASC or ADHD symptoms
- Postnatal Exposure- No significant associations were found for ASC or ADHD
- Covariates: Maternal characteristics included age at delivery (years), education (low, medium, high), pre-pregnancy body-mass index (BMI), alcohol (yes/no), smoking (yes/no) and mental health problems (yes/no) during pregnancy, age at birth (years) and parity (nulliparous, > 1 and > 2), maternal fever (yes/no) and infections (yes/no) during pregnancy. Maternal education was not provided by the DNBC and analyses were adjusted by maternal socio-occupational status based on job titles instead. Child characteristics included sex, age at behavioural assessment (years), cold (yes/no) and respiratory infections (yes/no) in the first 2 years of life.
- Autism Spectrum Condition (ASC)
Cohort Studies
- Streissguth, A. P., Treder, R. P., Barr, H. M., Shepard, T. H., Bleyer, W. A., Sampson, P. D., & Martin, D. C. (1987). Aspirin and acetaminophen use by pregnant women and subsequent child IQ and attention decrements. Teratology, 35(2), 211–219. https://doi.org/10.1002/tera.1420350207
- No significant findings for IQ or attention
- Autism symptoms or diagnosis not assessed
- Brandlistuen, R. E., Ystrom, E., Nulman, I., Koren, G., & Nordeng, H. (2013). Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. International journal of epidemiology, 42(6), 1702–1713. https://doi.org/10.1093/ije/dyt183
- Same-Sex Sibling Pairs, Discordant on use <28 days
- Psychomotor Problems
- Motor Milestone- .12 Beta coefficient
- Adjusted analysis- .10 Beta
- Gross Motor- .11 Beta
- Adjusted analysis- .10 Beta
- Fine Motor- .08 Beta
- Adjusted analysis- .07 Beta
- Communication- .04 Beta
- Adjusted analysis- .05 Beta
- Motor Milestone- .12 Beta coefficient
- Behavior Problems
- Externalizing- .08 Beta
- Temperament Problems
- Emotionality- .08 Beta
- Psychomotor Problems
- Same-Sex Sibling Pairs, Discordant on use equal or >28 days
- Psychomotor Problems
- Motor Milestone- .24 Beta
- Adjusted analysis- .26 Beta
- Gross Motor- .31 Beta
- Adjusted analysis- .24 Beta
- Communication- .22 Beta
- Adjusted analysis- .20 Beta
- Motor Milestone- .24 Beta
- Behavior Problems
- Externalizing- .24 Beta
- Adjusted analysis- .24 Beta
- Internalizing- .14 Beta
- Adjusted analysis- .14 Beta
- Externalizing- .24 Beta
- Temperament Problems
- Activity-.23 Beta
- Adjusted analysis- .22 Beta
- Activity-.23 Beta
- Psychomotor Problems
- Exposed vs. Non-Exposed in the Total Cohort, Exposure <28 days
- Psychomotor problems
- Gross Motor-.02 Beta
- Adjusted analysis- .03 Beta
- Communication-.03 Beta
- Gross Motor-.02 Beta
- Behavior Problems
- Externalizing-.09 Beta
- Adjusted analysis- .05 Beta
- Internalizing- .03 Beta
- Externalizing-.09 Beta
- Temperament Problems
- Emotionality- .06 Beta
- Adjusted analysis- .04 Beta
- Emotionality- .06 Beta
- Psychomotor problems
- Exposed vs. Non-Exposed in the Total Cohort, Exposure equal or >28 days
- Psychomotor problems
- Motor Milestone- .10 Beta
- Adjusted analysis- .08 Beta
- Gross Motor, adjusted analysis- .05 Beta
- Communication-.08 Beta
- Adjusted analysis- .08 Beta
- Motor Milestone- .10 Beta
- Behavior Problems
- Externalizing- .18 Beta
- Adjusted analysis- .13 Beta
- Internalizing- .08 Beta
- Externalizing- .18 Beta
- Temperament Problems
- Emotionality- .12 Beta
- Adjusted analysis- .10 Beta
- Emotionality- .12 Beta
- Psychomotor problems
- Other findings worth noting
- No difference between siblings discordant for first pregnancy exposure compared with second pregnancy exposure.
- No interaction effect between trimester and exposure on any of the outcomes
- No association between ibuprofen and neurodevelopmental outcomes
- Covariates: infections (respiratory, urinary tract/bladder, genital, diarhea/gastric flu), fever, back pain and headache or migraine; concomitant use of non-steroidal anti-inflammatory drugs (NSAIDs) (M01A and N02BA), triptans (N02CC), opioids (N02A), other analgesics (N02CA and N02CX), benzodiazepines (N05CD, N05BA), antidepressants (N06A), antipsychotics (N05A) and anti-epileptic drugs (N03A) was recorded and grouped as co-medication; mothers also reported on their psychological distress (anxiety and depression); maternal age at delivery, years between pregnancies, parity, smoking during pregnancy and alcohol use during pregnancy.
- Same-Sex Sibling Pairs, Discordant on use <28 days
- Liew, Z., Ritz, B., Rebordosa, C., Lee, P. C., & Olsen, J. (2014). Acetaminophen use during pregnancy, behavioral problems, and hyperkinetic disorders. JAMA pediatrics, 168(4), 313–320. https://doi.org/10.1001/jamapediatrics.2013.4914
- Hyperkinetic Disorders Hospital Diagnosis
- Never had psychiatric illness
- Ever used- 1.28x Adjusted Hazard Ratio
- In all 3 trimesters- 1.48x Adjusted Hazard Ratio
- No fever, inflammation and infections during pregnancy
- Ever used- 1.37x Adjusted Hazard Ratio
- In all 3 trimesters- 1.56x Adjusted Hazard Ratio
- No disease in muscles and joints during pregnancy
- Ever used- 1.25x Adjusted Hazard Ratio
- In all 3 trimesters- 1.4x Adjusted Hazard Ratio
- Never had psychiatric illness
- ADHD Medication Redemption
- Never had psychiatric illness
- Ever used- 1.21x Adjusted Hazard Ratio
- In all 3 trimesters- 1.47x Adjusted Hazard Ratio
- No fever, inflammation and infections during pregnancy
- Ever used- 1.3x Adjusted Hazard Ratio
- In all 3 trimesters- 1.41x Adjusted Hazard Ratio
- No disease in muscles and joints during pregnancy
- Ever used- 1.23x Adjusted Hazard Ratio
- In all 3 trimesters- 1.35x Adjusted Hazard Ratio
- Never had psychiatric illness
- Model A: adjusted maternal age at birth, gender of child, child’s birth year, gestational age, birth weight, parity, socio-economic status of mother, maternal smoking and alcohol drinking during pregnancy, maternal pre-pregnancy body mass index, and maternal diseases in muscles/joints, fever, or infection/inflammation during pregnancy.
- Ever used- 1.4x Adjusted Hazard Ratio
- All 3 trimesters- 1.66x Adjusted Hazard Ratio
- Model B: adjusted all in a plus maternal use of ibuprofen and aspirin during pregnancy.
- Ever used- 1.39x Adjusted Hazard Ratio
- All 3 trimesters- 1.65x Adjusted Hazard Ratio
- Model C: adjusted all in a plus mother’s ever had depression, anxiety, childhood psychiatric disorder, family problems/life crisis, or other mental health problems.
- Ever used- 1.37x Adjusted Hazard Ratio
- All 3 trimesters- 1.61x Adjusted Hazard Ratio
- Weeks of acetaminophen use during pregnancy
- 1 week- 1.35x Adjusted Hazard Ratio
- 2-5 weeks- 1.28x Adjusted Hazard Ratio (CI 1.00-1.64)
- 6-10 weeks- 1.72x Adjusted Hazard Ratio
- 11-20 weeks- 1.77x Adjusted Hazard Ratio
- >20 weeks- 2.06x Adjusted Hazard Ratio
- Covariates: child’s birth year, birth weight, and sex, as well as maternal age at child’s birth, parity, gestational age at delivery, socioeconomic status, smoking and alcohol drinking during pregnancy, pre-pregnancy body mass index (calculated as weight in kilograms divided by height in meters squared), and mother’s self-reported psychiatric illnesses; muscle and joint diseases, fever, and inflammation or infections.
- Hyperkinetic Disorders Hospital Diagnosis
- Thompson, J. M., Waldie, K. E., Wall, C. R., Murphy, R., Mitchell, E. A., & ABC study group (2014). Associations between acetaminophen use during pregnancy and ADHD symptoms measured at ages 7 and 11 years. PloS one, 9(9), e108210. https://doi.org/10.1371/journal.pone.0108210
- Strengths and Difficulties Questionnaire (ADHD symptoms)
- Parent form, age 7- 1.2 Mean Difference
- Parent form, age 11- .8 Mean Difference
- Child form, age 11 (child form)- .9 Mean Difference
- Parent Form, age 7
- Total Difficulties- 1.1 Multivariable (adjusted for confounders) Difference
- Emotion- .4 Multivariable Difference
- Conduct- .2 Multivariable Difference
- Parent Form, age 11
- Emotion- .5 Multivariable Difference
- Child Form, age 11
- Total Difficulties- 1.1 Multivariable Difference
- Conduct- .3 Multivariable Difference
- Hyperactivity- .4 Multivariable Difference
- Connors Behavioral Rating Scale (ADHD symptoms)
- Parent form, age 7
- CGI Emotional lability- 3.0 Multivariable Difference
- GI total- 2.6 Multivariable Difference
- DSM IV- Hyperactive impulsive- 2.0 Multivariable Difference
- DSM hyperactive-impulsive symptoms- .2 Multivariable Difference
- Parent form, age 11
- No significant findings after adjustment for covariates
- Parent form, age 7
- Covariates: SGA status, sex, age mother left school, maternal smoking during pregnancy, paternal smoking during pregnancy, marital status at birth, parity, socio- economic status, maternal pre-pregnancy BMI, maternal stress in the last month of pregnancy, alcohol consumption in the first trimester, living with the child’s biological father at 3.5 and child activity levels at 3.5, high fever during pregnancy, visiting GP for psychological conditions including depression and anxiety, taking medication during pregnancy for psychological conditions.
- Strengths and Difficulties Questionnaire (ADHD symptoms)
- Avella-Garcia, C. B., Julvez, J., Fortuny, J., Rebordosa, C., García-Esteban, R., Galán, I. R., Tardón, A., Rodríguez-Bernal, C. L., Iñiguez, C., Andiarena, A., Santa-Marina, L., & Sunyer, J. (2016). Acetaminophen use in pregnancy and neurodevelopment: attention function and autism spectrum symptoms. International journal of epidemiology, 45(6), 1987–1996. https://doi.org/10.1093/ije/dyw115
- ADHD-DSM-IV Total Symptoms
- Hyperactivity/impulsivity symptoms- 1.41x Adjusted Incidence Rate Ratio
- Kiddie Continuous Performance Test (K-CPT)
- Omission Errors (the child fails to respond to a presented stimulus)- 0.76x Incidence Rate Ratio
- Commission Errors (the child responds to a non-target stimulus)- 1.12x Incidence Rate Ratio
- Adjusted for covariates- 1.10 Adjusted Incidence Rate Ratio
- Hit Reaction Time Standard Error (HRT-SE)- -0.07 beta
- Detectability- -0.09 beta
- Detectability, adjusted for covariates- -0.08 beta
- Childhood Autism Spectrum Test (CAST)
- Males, adjusted for covariates- 0.63 beta
- Females- -0.63 beta
- Females, adjusted for covariates- -0.51 beta
- Dose-Response Analysis
- K-CPT
- HRT-SE
- All Participants + Persistent Use- 0.18 beta
- Males, Persistent Use- 0.22 beta
- Omission Errors
- All Participants + Persistent Use- 1.29x Incidence Rate Ratio
- Males + Persistent Use- 1.56x Incidence Rate Ratio
- Commission Errors
- All Participants + Sporadic Use- 1.1x Incidence Rate Ratio
- Females + Sporadic Use- 1.14x Incidence Rate Ratio
- Females + Persistent Use- 1.32 Incidence Rate Ratio
- Detectability
- All Participants + Sporadic Use- -0.08 beta
- Males + Persistent Use- 0.21 beta
- Females + Sporadic Use- -0.10 beta
- HRT-SE
- CAST
- Males + Sporadic Use- 0.56 beta
- Males + Persistent Use- 1.91 beta
- Females + Sporadic Use- -0.54 beta
- K-CPT
- Covariates: region, child gender, age at testing, gestational age at birth, quality of test as rated by the performing psychologist-only for BSID and MSCA, maternal social class, IQ, education and whether the mother reported having any chronic illness, fever or urinary tract infection-not necessarily related to acetaminophen use during pregnancy; for outcomes at 1 year of age, child age at testing was adjusted for prematurity); reported maternal chronic illness, fever or urinary tract infections at any time during pregnancy in all models.
- ADHD-DSM-IV Total Symptoms
- Stergiakouli, E., Thapar, A., & Davey Smith, G. (2016). Association of Acetaminophen Use During Pregnancy With Behavioral Problems in Childhood: Evidence Against Confounding. JAMA pediatrics, 170(10), 964–970. https://doi.org/10.1001/jamapediatrics.2016.1775
- Use at 18 weeks of pregnancy
- Conduct Problems- 1.2x Risk Ratio
- Adjusted for postnatal use- 1.18x Risk Ratio
- Adjusted for partner’s use- 1.39x Risk Ratio
- Hyperactivity Problems- 1.23x Risk Ratio
- Adjusted for postnatal use- 1.21x Risk Ratio
- Adjusted for partner’s use- 1.27x Risk Ratio
- SDQ Total Difficulties, adjusted for partner’s use- 1.41x Risk Ratio
- Conduct Problems- 1.2x Risk Ratio
- Use at 32 weeks of pregnancy
- SDQ Total Difficulties- 1.46x Risk Ratio
- Adjusted for postnatal use- 1.47x Risk Ratio
- Adjusted for partner’s use- 1.85x Risk Ratio
- Emotional Symptoms- 1.29x Risk Ratio
- Adjusted for postnatal use- 1.24x Risk Ratio
- Conduct Problems- 1.42x Risk Ratio
- Adjusted for postnatal use- 1.4x Risk Ratio
- Adjusted for partner’s use- 1.53x Risk Ratio
- Hyperactivity Symptoms- 1.31x Risk Ratio
- Adjusted for postnatal use- 1.34x Risk Ratio
- Adjusted for partner’s use- 1.43x Risk Ratio
- SDQ Total Difficulties- 1.46x Risk Ratio
- No significant findings for postnatal use
- Use at 18 weeks of pregnancy
- Liew, Z., Ritz, B., Virk, J., & Olsen, J. (2016). Maternal use of acetaminophen during pregnancy and risk of autism spectrum disorders in childhood: A Danish national birth cohort study. Autism research : official journal of the International Society for Autism Research, 9(9), 951–958. https://doi.org/10.1002/aur.1591
- Autism Spectrum Disorders
- Ever used- 1.19x Adjusted Hazard Ratio
- Both first and second trimester- 1.38x Adjusted Hazard Ratio
- All three trimesters- 1.39x Adjusted Hazard Ratio
- Infantile autism- 1.49x Adjusted Hazard Ratio
- 2-5 weeks of use- 1.23x Adjusted Hazard Ratio
- >20 weeks of use- 1.54x Adjusted Hazard Ratio
- Infantile autism- 1.62x Adjusted Hazard Ratio
- Autism Spectrum Disorders
- Without hyperkinetic symptoms
- >20 weeks of use- 1.42x Adjusted Hazard Ratio
- With hyperkinetic symptoms
- Ever used- 1.51x Adjusted Hazard Ratio
- All three trimesters- 1.77x Adjusted Hazard Ratio
- Infantile autism- 2.45x Adjusted Hazard Ratio
- 1-5 weeks of use- 1.51x Adjusted Hazard Ratio
- 6-20 weeks of use- 1.62x Adjusted Hazard Ratio
- >20 weeks- 1.89x Adjusted Hazard Ratio
- Without hyperkinetic symptoms
- Covariates: child’s sex, birth year, maternal age at birth, parity, socioeconomic status, maternal smoking and alcohol drinking during pregnancy, maternal prepregnancy body mass index, folic acid intake during pregnancy, mother’s psychiatric illnesses, maternal diseases in muscles/joints, fever, or infection/inflammation during pregnancy, maternal use of ibuprofen and aspirin during pregnancy.
- Autism Spectrum Disorders
- Ji, Y., Azuine, R. E., Zhang, Y., Hou, W., Hong, X., Wang, G., Riley, A., Pearson, C., Zuckerman, B., & Wang, X. (2020). Association of Cord Plasma Biomarkers of In Utero Acetaminophen Exposure With Risk of Attention-Deficit/Hyperactivity Disorder and Autism Spectrum Disorder in Childhood. JAMA psychiatry, 77(2), 180–189. https://doi.org/10.1001/jamapsychiatry.2019.3259
- Cord Unchanged Acetaminophen, Third Tertile
- ADHD- 2.88x Adjusted Odds Ratio
- ASD- 3.72x Adjusted Odds Ratio
- ADHD and ASD- 3.38x Adjusted Odds Ratio
- Cord Acetaminophen Glucuronide, Any detection
- ADHD- 2.25x Adjusted Odds Ratio
- ASD- 2.29x Adjusted Odds Ratio
- Cord 3-(N-Acetyl-L-Cystein-S-yl)-Acetaminophen, Any detection
- ADHD- 1.69x Adjusted Odds Ratio
- Cord Acetaminophen Burden
- ADHD, Second tertile- 2.26x Adjusted Odds Ratio
- ADHD, Third tertile- 2.86x Adjusted Odds Ratio
- ASD, Third tertile- 3.62x Adjusted Odds Ratio
- Covariates: maternal age at delivery, maternal race/ethnicity, maternal educational level, marital status, stress during pregnancy, smoking before or during pregnancy, alcohol use before or during pregnancy, maternal body mass index, parity, child’s sex, delivery type, preterm birth, and low birth weight.
- Autism Librarian’s note: Maternal fever during pregnancy was not significantly associated with risk of ADHD or autism in this study, eliminating the need for the authors to conduct analyses for confounding by indication.
- Autism Librarian’s note: I would’ve also like to have seen data collected on maternal usage of acetaminophen during the various trimesters and analyses conducted on the trimester impact on the Cord Plasma Biomarkers to answer the question of: which trimester of exposure to acetaminophen results in the greatest impact to these biomarkers?
- Cord Unchanged Acetaminophen, Third Tertile
- Ahlqvist, V. H., Sjöqvist, H., Dalman, C., Karlsson, H., Stephansson, O., Johansson, S., Magnusson, C., Gardner, R. M., & Lee, B. K. (2024). Acetaminophen Use During Pregnancy and Children’s Risk of Autism, ADHD, and Intellectual Disability. JAMA, 331(14), 1205–1214. https://doi.org/10.1001/jama.2024.3172
- Population model adjusted for birth cohort; child sex; all other analgesics; birthing parent’s diagnoses of migraine, chronic pain, infections, fevers, rheumatoid arthritis, and headaches; calendar period of delivery; parity; age at delivery (linear and cubic term); country of birth; residential region; cohabitation at delivery; early pregnancy body mass index; smoking status; diagnosis of autism, attention-deficit/hyperactivity disorder (ADHD), and intellectual disability; history of psychiatric conditions and prescription use of psycholeptics, antidepressants, and antiseizure medication; health care visits in the year before pregnancy and an inadequate number of antenatal visits; and the highest household education and disposable income.
- Autism, population model
- Acetaminophen- 1.05x Hazard Ratio
- Non-Aspirin NSAIDs- 1.07x Hazard Ratio
- Opioids- 1.15x Hazard Ratio
- Anti-migraine- 1.17x Hazard Ratio
- ADHD, population model
- Acetaminophen- 1.07x Hazard Ratio
- Non-Aspirin NSAIDs- 1.1x Hazard Ratio
- Opioids- 1.23x Hazard Ratio
- Anti-migraine- 1.12 Hazard Ratio
- Autism, population model
- The sibling control model was adjusted for all of the above excluding birthing parent’s birth country, psychiatric history, and diagnosis autism, ADHD, and intellectual disability.
- Autism, siblings model
- Aspirin- .87x Hazard Ratio
- ADHD, siblings model
- No significant findings
- Intellectual Disability, siblings and population
- No significant findings for population analyses
- Aspirin, siblings- .71x Hazard Ratio
- Autism, siblings model
- Model 1: adjusted for birth cohort and child sex
- Autism, low dose- 1.33x Adjusted Hazard Ratio
- Autism, medium dose- 1.52x Adjusted Hazard Ratio
- Autism, high dose- 1.87x Adjusted Hazard Ratio
- ADHD, low dose- 1.46x Adjusted Hazard Ratio
- ADHD, medium dose- 1.75x Adjusted Hazard Ratio
- ADHD, high dose- 1.97x Adjusted Hazard Ratio
- Intellectual disability, low dose- 1.34x Adjusted Hazard Ratio
- Intellectual disability, medium dose- 1.47x Adjusted Hazard Ratio
- Intellectual disability, high dose- 1.92x Adjusted Hazard Ratio
- Model 2: Model 1 plus birthing parent’s diagnosis of migraine, chronic pain, infections, fevers, rheumatoid arthritis, and headaches, and any other analgesics (aspirin, nonaspirin NSAIDs, opioids, or anti-migraine medications)
- Autism, low dose- 1.14x Adjusted Hazard Ratio
- Autism, medium dose- 1.29x Adjusted Hazard Ratio
- Autism, high dose- 1.45x Adjusted Hazard Ratio
- ADHD, low dose- 1.17x Adjusted Hazard Ratio
- ADHD, medium dose- 1.39x Adjusted Hazard Ratio
- ADHD, high dose- 1.41x Adjusted Hazard Ratio
- Intellectual disability, low dose- 1.27x Adjusted Hazard Ratio
- Intellectual disability, medium dose- 1.38x Adjusted Hazard Ratio
- Intellectual disability, high dose- 1.75x Adjusted Hazard Ratio
- Model 3: Model 2 plus calendar period of delivery, parity, birthing parent’s age at delivery, country of birth, residential region, cohabitation at delivery, early pregnancy body mass index, smoking status, and birthing parent’s autism, ADHD, intellectual disability, history of psychiatric conditions, and birthing parent’s prescription use of psycholeptic medications, antidepressants, and antiseizure medication, and health care visits in the year before pregnancy, and an inadequate number of antenatal visits, and the highest household education and disposable income.
- Autism, medium dose- 1.11x Adjusted Hazard Ratio
- ADHD, medium dose- 1.25x Adjusted Hazard Ratio
- ADHD, high dose- 1.17x Adjusted Hazard Ratio
- No significant findings for intellectual disability under model 3 adjustments
- Sibling analysis: model 3 covariates, excluding those with perfect balance between full siblings (ie, birthing parent’s birth country, psychiatric history, and diagnosis of autism, ADHD, and intellectual disability).
- No significant findings
- Autism Librarian’s note: was adjusting for the following covariates appropriate? Did the inclusion of these covariates remove significant associations via the removal of any variance collectively associated with each of these covariates?
- Residential region- 13 out of 30 significant associations on autism, ADHD, and intellectual disability; is this enough to justify including it as a covariate?
- Adjusted for this in their Model 3 and Sibling Analysis
- Early-pregnancy BMI category- 8 out of 24 associations on autism, ADHD, and intellectual disability are significant; is this enough to justify including it as a covariate?
- Adjusted for this in their Model 3 and Sibling Analysis
- Chronic pain- 1 out of 6 associations on autism, ADHD, and intellectual disability are significant; is this enough to justify including it as a covariate?
- Adjusted for this in their Model 2, Model 3, and Sibling Analysis
- Migraine- zero significant odds ratios for autism, ADHD, or intellectual disability
- Adjusted for this in their Model 2, Model 3, and Sibling Analysis
- Fever- zero significant odds ratios for autism, ADHD, or intellectual disability
- Adjusted for this in their Model 2, Model 3, and Sibling Analysis. This one is kind of huge because maternal fever is common reason for using acetaminophen…
- Rheumatoid arthritis- zero significant odds ratios for autism, ADHD, or intellectual disability
- Authors adjusted for this in their Model 2, Model 3, and Sibling Analysis
- Psycholeptics medications- zero significant odds ratios for autism, ADHD, or intellectual disability
- Authors adjusted for this in their Model 3 and Sibling Analysis
- Residential region- 13 out of 30 significant associations on autism, ADHD, and intellectual disability; is this enough to justify including it as a covariate?
- Population model adjusted for birth cohort; child sex; all other analgesics; birthing parent’s diagnoses of migraine, chronic pain, infections, fevers, rheumatoid arthritis, and headaches; calendar period of delivery; parity; age at delivery (linear and cubic term); country of birth; residential region; cohabitation at delivery; early pregnancy body mass index; smoking status; diagnosis of autism, attention-deficit/hyperactivity disorder (ADHD), and intellectual disability; history of psychiatric conditions and prescription use of psycholeptics, antidepressants, and antiseizure medication; health care visits in the year before pregnancy and an inadequate number of antenatal visits; and the highest household education and disposable income.
Case Control Studies
- Schultz, S. T., Klonoff-Cohen, H. S., Wingard, D. L., Akshoomoff, N. A., Macera, C. A., & Ji, M. (2008). Acetaminophen (paracetamol) use, measles-mumps-rubella vaccination, and autistic disorder: the results of a parent survey. Autism: the international journal of research and practice, 12(3), 293–307. https://doi.org/10.1177/1362361307089518
- Crude Associations
- Presence of illness concurrent with MMR- 11.5x Odds Ratio
- No. sequelae to MMR- 2.36x Odds Ratio
- Acetaminophen use after MMR- 2.42x Odds Ratio
- Acetaminophen use age 12–18 months- 5.42x Odds Ratio
- Acetaminophen use at age 12 to 18 months– adjusted for age, gender, and mother’s ethnicity
- Children 1-18 years- 8.37x Adjusted Odds Ratio
- Children 1–18 years, cases limited to children with regression- 20.9x Adjusted Odds Ratio
- Association of presence of illness concurrent with MMR vaccine and autism- adjusted for age, gender, mother’s ethnicity, and acetaminophen use after measles-mumps-rubella vaccination
- Children 1-18 years- 8.81x Adjusted Odds Ratio
- Children 1–18 years, cases limited to children with regression- 17.2x Adjusted Odds Ratio
- Analgesic use after MMR vaccine- adjusted for age, gender, mother’s ethnicity, and acetaminophen use after measles-mumps-rubella vaccination.
- Acetaminophen
- Children 1-5 years- 6.11x Adjusted Odds Ratio
- Children 1–18 years, cases limited to children with regression- 3.97x Adjusted Odds Ratio
- Children 1–18 years with post-vaccination sequelae- 8.23x Adjusted Odds Ratio
- Ibuprofen- no significant findings
- Acetaminophen
- No effect found for interaction with the number of post-vaccination sequelae and with the presence of concurrent illness at the time of the MMR vaccination.
- Average age of children
- Age: mean (SD) (years) for Cases- N = 83, 7.7 (4.1)
- Age: mean (SD) (years) for Controls- N = 80, 7.3 (3.9)
- Autism Librarian’s note: this is one of the few studies on postnatal exposure to acetaminophen specifically after a vaccine, perhaps the only study. More studies such as this are needed.
- Crude Associations
- Schultz, S. T., & Gould, G. G. (2016). Acetaminophen Use for Fever in Children Associated with Autism Spectrum Disorder. Autism-open access, 6(2), 170. https://doi.org/10.4172/2165-7890.1000170
- Acetaminophen, first choice of medicine- 83% less likely to have autism, 0.165 Odds Ratio
- Use of acetaminophen if other medication doesn’t bring down fever- 82% less likely to have autism, 0.183 Odds Ratio
- Significantly higher number of children with autism used ibuprofen to bring down their fever vs. rarely or never using ibuprofen if acetaminophen does not bring down their fever.
- Average age of children
- Age (months) for Cases- N = 118, 131.3 (43.6)
- Age (months) for Controls- N = 79, 134.9 (39.6)
- Regarding the findings, the authors had this to say: “If we consider that early use of acetaminophen may be responsible for endocannabinoid system dysfunction, this could result in acetaminophen losing effectiveness. In this case, the results we found in older children are to be expected.”
- Siniscalco, D., Sapone, A., Giordano, C., Cirillo, A., de Magistris, L., Rossi, F., Fasano, A., Bradstreet, J. J., Maione, S., & Antonucci, N. (2013). Cannabinoid receptor type 2, but not type 1, is up-regulated in peripheral blood mononuclear cells of children affected by autistic disorders. Journal of autism and developmental disorders, 43(11), 2686–2695. https://doi.org/10.1007/s10803-013-1824-9
- Bittker, S. S., & Bell, K. R. (2018). Acetaminophen, antibiotics, ear infection, breastfeeding, vitamin D drops, and autism: an epidemiological study. Neuropsychiatric disease and treatment, 14, 1399–1414. https://doi.org/10.2147/NDT.S158811
- Duration of Breastfeeding
- Never breastfed- 1.935x Odds Ratio
- 3 months or less- 2.076x Odds Ratio
- >12 months- .407 Odds Ratio
- Breastfeeding (months)- .935x Odds Ratio
- Breastfeeding (months)- .948x Adjusted Odds Ratio
- Courses of Antibiotics up to second birthday
- None- .667x Odds Ratio
- 1- .638 Odds Ratio
- 4-7- 1.642x Odds Ratio
- 8-15- 2.086 Odds Ratio
- Antibiotic (courses)- 1.138x Odds Ratio
- Antibiotic (courses)- 1.103x Adjusted Odds Ratio
- Ear infections up to second birthday
- None- .644x Odds Ratio
- 1- .764 Odds Ratio
- 2-3- 1.533 Odds Ratio
- >3 or persistent- 1.694x Odds Ratio
- Ear infection (number)- 1.208x Odds Ratio
- Ear infection (number)- 1.137x Adjusted Odds Ratio
- Doses of acetaminophen up to second birthday
- None- .652x Odds Ratio
- 64+- 3.743x Odds Ratio
- Acetaminophen (doses)- 1.015x Odds Ratio
- Acetaminophen (doses)- 1.016x Adjusted Odds Ratio
- Duration of vitamin D drops as a baby
- No vitamin D drops- 1.475x Odds Ratio
- 3 months or less- .646x Odds Ratio
- Dosage of vitamin D drops as a baby
- No vitamin D drops- 1.489x Odds Ratio
- Less than the standard dose- .376 Odds Ratio
- About the standard dose- .738x Odds Ratio
- Specialized General Linear Models
- Antibiotic/Ear infection- 1.080 Adjusted Odds Ratio
- Low-granularity antibiotic/Ear Infection- 1.177x Adjusted Odds Ratio
- Breastfeeding/Vitamin D drops- .948x Adjusted Odds Ratio
- Breastfeeding/Vitamin D drops excluding >1 ASD child- .949x Adjusted Odds Ratio
- Breastfeeding/Total vitamin D- .963x Adjusted Odds Ratio
- Multifactor Model
- Breastfeeding (months)- .954x Adjusted Odds Ratio
- Antibiotic (course) 1.083x Adjusted Odds Ratio
- Gender (male)- 3.951x Adjusted Odds Ratio
- No significant findings regarding folate supplementation
- Covariates: gender, age of the child, ethnicity, Midwest, South, maternal education, age of the mother at the birth of the child, and relationship
- Duration of Breastfeeding
- Saunders, A., Woodland, J., & Gander, S. (2019). A Comparison of Prenatal Exposures in Children with and without a Diagnosis of Autism Spectrum Disorder. Cureus, 11(7), e5223. https://doi.org/10.7759/cureus.5223
- No significant findings regarding acetaminophen
- Estimated Gestational Age at Start of Prenatal Vitamins- 2.981 Independent t-test, with ASD group being higher
- Chi-Square Tests
- Sibling with ASD- 13.189 X2
- Family member with ASD- 14.89 X2
- Medication use- 9.557 X2
- Cigarette use- 19.679 X2
- Logistic Regression
- ASD Family- 2.72x Odds Ratio
- Medications- 2.29x Odds Ratio
- Smoking- 2.56x Odds Ratio
Other Designs
- Bauer, A. Z., & Kriebel, D. (2013). Prenatal and perinatal analgesic exposure and autism: an ecological link. Environmental health : a global access science source, 12, 41. https://doi.org/10.1186/1476-069X-12-41
- Country’s average prenatal paracetamol consumption was found to be correlated with its autism/ASD prevalence- r = 0.80
- Country level data between circumcision and autism spectrum disorder- r =0.98
Animal Studies
- Viberg, H., Eriksson, P., Gordh, T., & Fredriksson, A. (2014). Paracetamol (acetaminophen) administration during neonatal brain development affects cognitive function and alters its analgesic and anxiolytic response in adult male mice. Toxicological sciences : an official journal of the Society of Toxicology, 138(1), 139–147. https://doi.org/10.1093/toxsci/kft329
- Brain-Derived Neurotrophic Factor (BDNF)- promotes neuronal survival but also regulates cell migration, axonal and dendritic outgrowth, and formation and function of synapses
- Male mice receiving multiple doses, 30 + 30mg paracetamol/kg bw
- BDNF increased significantly 183% in frontal cortex; a significant decrease of 26% in parietal cortex
- Spontaneous Behavior in 2-Month Old Male Mice
- Locomotion, rearing, and total activity significantly decreased
- Radial Arm Maze Learning in 2-Month-Old Male Mice
- Significantly longer time finding all 8 food pellets; significantly more errors on test days 2 and 3
- Hot Plate Test in 3-Month-Old Male Mice
- Significantly shorter time on the hot plate than control group
- Dose-Response Effect: Animals neonatally exposed to double doses spent significantly shorter time on the hot plate than control group and group exposed only once
- Elevated Plus Maze in 3-Month-Old Male Mice
- Control group: percent of time spent in the open arms and entries into the open arms increased significantly
- Animals exposed with double doses spent significantly shorter time and made fewer entries into th eopen arms than the control group
- Animals exposed to single dose spent significantly less time in the open arms compared to control group
- Philippot, G., Gordh, T., Fredriksson, A., & Viberg, H. (2017). Adult neurobehavioral alterations in male and female mice following developmental exposure to paracetamol (acetaminophen): characterization of a critical period. Journal of applied toxicology: JAT, 37(10), 1174–1181. https://doi.org/10.1002/jat.3473
- Male mice
- Postnatal day 3 and day 10 exposure to paracetamol
- Significantly different from controls for locomotion, rearing, and total activity during the first 20 minutes of testing.
- Significant increase in locomotion and rearing during last 20 minutes of testing
- Postnatal day 19
- No significant changes
- Postnatal day 3 and day 10 exposure to paracetamol
- Female mice
- No significant differences in locomotion, rearing, or male vs. female habituation quotients of control mice
- Male mice
- Blecharz-Klin, K., Wawer, A., Jawna-Zboińska, K., Pyrzanowska, J., Piechal, A., Mirowska-Guzel, D., & Widy-Tyszkiewicz, E. (2018). Early paracetamol exposure decreases brain-derived neurotrophic factor (BDNF) in striatum and affects social behaviour and exploration in rats. Pharmacology, biochemistry, and behavior, 168, 25–32. https://doi.org/10.1016/j.pbb.2018.03.004
- Paracetamol exposed rats had significantly less social interactions and sniffing behaviors
- 15mg/kg paracetamol exposed rats had significantly increased pinning behaviors
- 15mg/kg paracetamol exposed rats had significantly increased total time exploring both objects during familiarization phase; and total time exploring all objects during both familiarization and choice phases
- Brain-Derived Neurotrophic Factor (BDNF)
- A two-fold decrease in BDNF in paracetamol-treated rats
- No differences in BDNF in prefrontal cortex, hippocampus, or between both treated groups
- Striatal BDNF concentration in control group correlated with sniffing behaviors
- No correlations between BDNF levels and any other parameters
- Suda, N., Cendejas Hernandez, J., Poulton, J., Jones, J. P., Konsoula, Z., Smith, C., & Parker, W. (2021). Therapeutic doses of acetaminophen with co-administration of cysteine and mannitol during early development result in long term behavioral changes in laboratory rats. PloS one, 16(6), e0253543. https://doi.org/10.1371/journal.pone.0253543
- Acetaminophen treatment plus antioxidant (cysteine and mannitol) treatment on days P4 through P10 resulted in significant increase in asocial behavior, rearing.
- Animals not receiving oxidative stress factors
- Early life treatment with acetaminophen plus the antioxidant cysteine had 38.4% more rearing behavior at age P37 through P49
- Animals receiving oxidative stress factors
- Treatment with acetaminophen plus the antioxidant cysteine had 50.6% more rearing behavior at age P37 through P49
- 2-Way ANOVA revealed no interaction effect on exposure to oxidative stress factors and treatment with acetaminophen- which means exposure to oxidative stress had no effect on the effect of the exposure of acetaminophen plus cysteine
- 2-Way ANOVA found significant effect of treatment with acetaminophen plus cysteine on rearing behavior; also a significant effect of the exposure of stress factors on rearing behavior
- Exposure to stress early in life was associated with a decrease in rearing behavior at age P37 and P49
- Herrington, J. A., Guss Darwich, J., Harshaw, C., Brigande, A. M., Leif, E. B., & Currie, P. J. (2022). Elevated ghrelin alters the behavioral effects of perinatal acetaminophen exposure in rats. Developmental psychobiology, 64(3), e22252. https://doi.org/10.1002/dev.22252
- Open Field Test
- Anxiety- related behaviors- Rats exposed to acetaminophen but not treated with ghrelin had more exploratory behavior than controls
- Anxiety- related behaviors- Rats treated with both acetaminophen and ghrelind did not differ from controls
- Anxiety- related behaviors-Female rats had lower levels of exploration than males
- Activity levels- Significantly lower activity levels during the second half of the open field test
- Activity levels- rats treated to acetaminophen but not treated with ghrelin
- Elevated Plus Maze
- Males had greater number of entries into the open arms than females
- No longer significant after ghrelin exposure
- Ghrelin treated rats showed higher levels of activity
- Males had greater number of entries into the open arms than females
- Open Field Test
- Harshaw, C., & Warner, A. G. (2022). Interleukin-1β-induced inflammation and acetaminophen during infancy: Distinct and interactive effects on social-emotional and repetitive behavior in C57BL/6J mice. Pharmacology, biochemistry, and behavior, 220, 173463. https://doi.org/10.1016/j.pbb.2022.173463
- Circling behavior
- Mice exposed to acetaminophen completed more 360 rotations than those unexposed in the marble burying test
- IL-1β plus acetaminophen exposed mice had more 360 rotations than mice that received only IL-1β
- Clockwise vs. counter-clockwise circling
- IL-1β exposed mice had fewer clockwise rotations compared to counterclockwise rotations
- Females treated with IL-1β early in life had lower clockwise rotations
- Mice treated with acetaminophen only showed more clockwise rotations than IL-1β plus acetaminophen during the second habituation trial
- Marble burying
- Early life exposure for mice treated with IL-1β engaged in less digging
- Center: edge ratio
- Acetaminophen treated mice had greater thigmotaxis (wall hugging)
- Mice exposed to both IL-1β plus acetaminophen had lower center:edge ratios than vehicles only exposed to IL-1β, and trended toward center:edge ratios than control group
- Females had significantly lower center:edge ratios than females exposed to either IL-1β or acetaminophen.
- Mice exposed to both IL-1β plus acetaminophen had lower center:edge ratios than mice only exposed to acetaminophen alone
- Other open field anxiety measures
- Rectal temperature- IL-1β treated females had Trectal values higher than both IL-1β exposed and control group males
- Maternal separation test (Ultrasonic Vocalizations- USVs)
- IL-1β exposed infant rodents produced more USVs than control group
- Close, non-social behaviors/avoidance
- Mice with early life exposure to acetaminophen displayed more close, non-social behavior/avoidance of the stimulus mouse than those unexposed
- IL-1β exposed males had less close, non-social behavior/avoidance than control group
- Acetaminophen exposed mice, and unexposed to IL-1β, had more avoidance than control group
- IL-1β exposed mice had longer bouts of avoidance than control
- Males treated with acetaminophen had longer bouts of avoidance than control group
- IL-1β plus acetaminophen exposed males had longer bouts of avoidance than males in all other conditions
- Following/anogenital sniffing
- Males with early life exposure to IL-1β had higher levels of following and anogenital sniffing than unexposed males
- Social Caution
- Males exposed to acetaminophen showed greater levels of caution (longer latencies for social behaviors) than unexposed
- Sociability-social novelty
- IL-1β exposed mice approached the mouse side more rapidly than control group
- IL-1β exposed mice were quicker to approach the mouse relative to the empty cage side
- Male mice were closer to the cage when on the stimulus mouse side than they were on the empty cage side in the control groups, as well as mice exposed to both IL-1β plus acetaminophen
- Females had differences in how close they were to the stimulus vs empty cage
- Social novelty phase
- Females exposed to acetaminophen had more entries to the familiar mouse side
- Circling behavior
- Baker, B. H., Rafikian, E. E., Hamblin, P. B., Strait, M. D., Yang, M., & Pearson, B. L. (2023). Sex-specific neurobehavioral and prefrontal cortex gene expression alterations following developmental acetaminophen exposure in mice. Neurobiology of disease, 177, 105970. https://doi.org/10.1016/j.nbd.2022.105970
- Pup ultrasonic vocalizations
- Increased ultrasonic vocalizations on postnatal day 8 among males
- Open Field Test
- Male mice had lower total ambulation in the open field test
- Decreased ambulatory movement in males in the first 10-minute time-bin of the open field test
- Decreased total rearings among offspring
- Cohort-stratified analyses
- Males had significantly lower total ambulation than the control
- RNA-Sequencing
- 10 altered genetic expressions in prefrontal cortex
- Enriched pathways from Ensemble of Gene Set Enrichment Analysis (EGSEA)
- Glutathione S-transferase
- Cytochrome p450 enzymes
- DNA damage
- Apoptosis
- Endocrine system
- Immune system
- Both male and female mice had effected pathways related to DNA damage and immune activation
- Upregulation of the estrogen response in females only
- Upregulation of autoimmune thyroid diseases in males only
- Upregulated pathways of metabolism of glutathione S-transferase and cytochrome p450 in females only
- Some DNA damage pathways upregulated in males only
- Pup ultrasonic vocalizations
2025 Lineup
- Ali, N. A., Kennon-McGill, S., Parker, L. D., James, L. P., Fantegrossi, W. E., & McGill, M. R. (2025). NAPQI is absent in the mouse brain after sub-hepatotoxic and hepatotoxic doses of acetaminophen. Toxicological sciences : an official journal of the Society of Toxicology, 205(2), 274–278. https://doi.org/10.1093/toxsci/kfaf034
Literature Reviews
- Parker, W., Hornik, C. D., Bilbo, S., Holzknecht, Z. E., Gentry, L., Rao, R., Lin, S. S., Herbert, M. R., & Nevison, C. D. (2017). The role of oxidative stress, inflammation and acetaminophen exposure from birth to early childhood in the induction of autism. The Journal of international medical research, 45(2), 407–438. https://doi.org/10.1177/0300060517693423
- Khan, F. Y., Kabiraj, G., Ahmed, M. A., Adam, M., Mannuru, S. P., Ramesh, V., Shahzad, A., Chaduvula, P., & Khan, S. (2022). A Systematic Review of the Link Between Autism Spectrum Disorder and Acetaminophen: A Mystery to Resolve. Cureus, 14(7), e26995. https://doi.org/10.7759/cureus.26995
- Kwok, J., Luedecke, E., Hall, H. A., Murray, A. L., & Auyeung, B. (2022). Analgesic drug use in pregnancy and neurodevelopment outcomes: an umbrella review. Neuroscience and biobehavioral reviews, 136, 104607. https://doi.org/10.1016/j.neubiorev.2022.104607
- Parker, W., Anderson, L. G., Jones, J. P., Anderson, R., Williamson, L., Bono-Lunn, D., & Konsoula, Z. (2023). The Dangers of Acetaminophen for Neurodevelopment Outweigh Scant Evidence for Long-Term Benefits. Children (Basel, Switzerland), 11(1), 44. https://doi.org/10.3390/children11010044
- Zhao, L., Jones, J. P., Anderson, L. G., Konsoula, Z., Nevison, C. D., Reissner, K. J., & Parker, W. (2024). Acetaminophen causes neurodevelopmental injury in susceptible babies and children: no valid rationale for controversy. Clinical and experimental pediatrics, 67(3), 126–139. https://doi.org/10.3345/cep.2022.01319
- Csoka, A. B., El Kouhen, N., Bennani, S., Getachew, B., Aschner, M., & Tizabi, Y. (2024). Roles of Epigenetics and Glial Cells in Drug-Induced Autism Spectrum Disorder. Biomolecules, 14(4), 437. https://doi.org/10.3390/biom14040437
- Jones, J. P., 3rd, Williamson, L., Konsoula, Z., Anderson, R., Reissner, K. J., & Parker, W. (2024). Evaluating the Role of Susceptibility Inducing Cofactors and of Acetaminophen in the Etiology of Autism Spectrum Disorder. Life (Basel, Switzerland), 14(8), 918. https://doi.org/10.3390/life14080918
- Statistically argued and presented evidence regarding the inappropriateness of the Cox regression analysis utilized by Ahlqvist et al. (2024) published in JAMA to conclude no association between prenatal acetaminophen exposure and autism after adjusting for various cofactors.
- “It is well established that cofactors or interacting variables should not be treated as independent variables when performing a Cox regression analysis.
That is to say, the Cox regression analysis can be used to determine whether acetaminophen or other factors cause ASD, but it cannot be used to determine if acetaminophen in combination with other factors cause ASD unless the parameters are adjusted accordingly.
Specifically, the [acetaminophen + other factors] interaction parameter must be included in the analysis. At the same time, underreporting of acetaminophen use and/or an abundance of acetaminophen use by individuals not at risk can also undermine the analysis.” - “The present study demonstrates clearly that, if the interaction of acetaminophen with a complex array of factors causes ASD, a multivariate analysis of cohort-derived data treating cofactors as confounding factors is of very limited usefulness.”